
- MEDI CAL TIMELY FILING LIMIT MANUALS
- MEDI CAL TIMELY FILING LIMIT VERIFICATION
- MEDI CAL TIMELY FILING LIMIT CODE
Non-Discrimination Policy and Accessibility Services.Get a Quote for Individual and Family PlansĪncillary and Specialty Benefits for Employees.Health Plans for Individuals and Families.
MEDI CAL TIMELY FILING LIMIT MANUALS
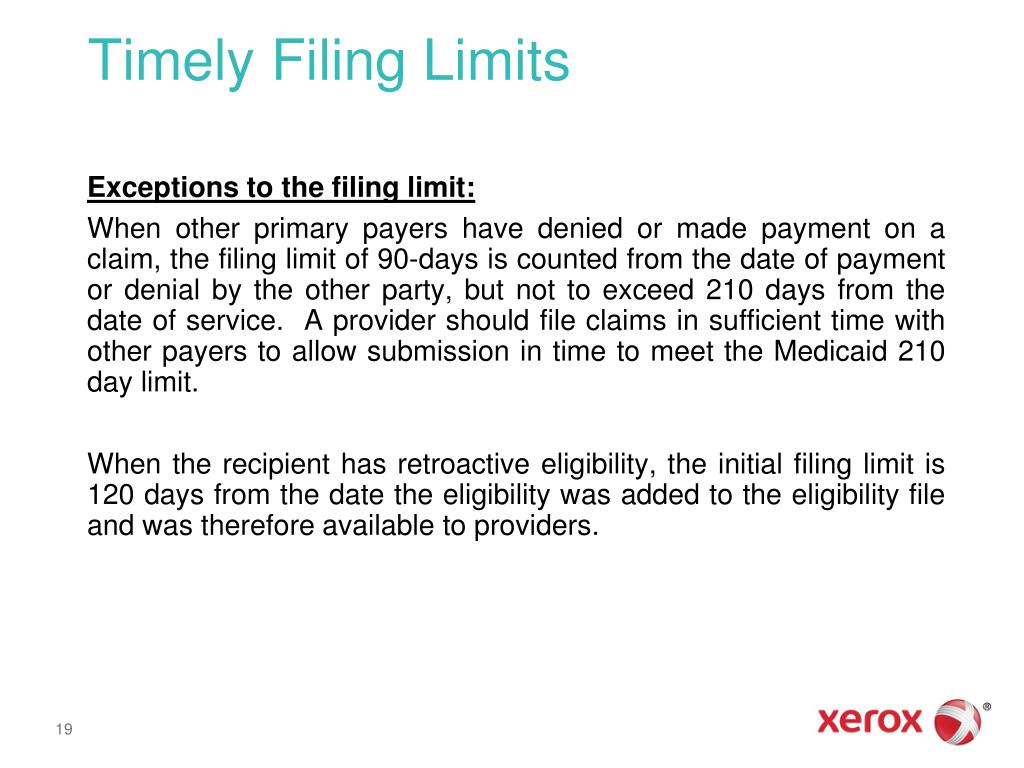
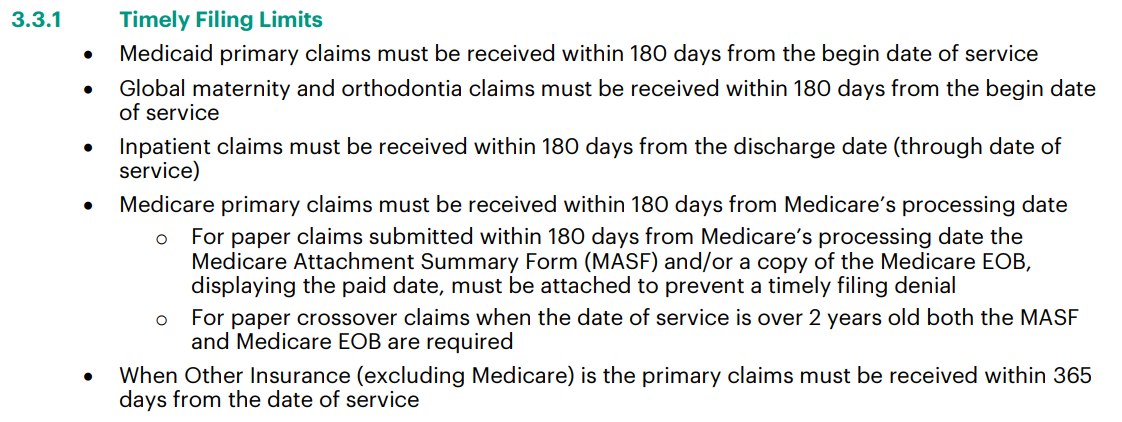
Refer to the billing manuals for a complete list of the codes.Īppeals of denied or paid claims must be submitted within 365 days from the original denial or paid dates. Place of Service Codes – Place of Service codes are two (2) digit nationally recognized codes. When submitting an Adjustment or Void, indicate the Transaction Control Number (TCN) from the most recent paid claim. Retroactive Eligibility – When a recipient receives retroactive eligibility, include an attachment indicating the recipient's retroactive eligibility. Timely filing guidelines for Medicare/Medicaid Crossover and third party claims are 180 days from the Medicare or third party payer's payment date.Ĭlaims filed within 365 days of the date of service that were denied for any reason other than timely filing may be resubmitted with a copy of the Remittance Advice (RA) indicating the original date of denial.Īdjustments may be submitted within 365 days of the paid date. Timely Filing TCN – Claims for covered services must be filed within 365 days from the date of service.
A missed appointment is not a distinct reimbursable Medicaid service but a part of the provider's overall cost of doing business.

Missed Appointments – According to the Centers for Medicare and Medicaid Services (CMS), providers are not allowed to bill recipients for missed appointments. TPL Denials - When the third-party payment source denies payment, you must attach the EOB statement of denial to the hardcopy claim or upload with the online submitted claim. Medicare Denials – When billing for services denied by Medicare for recipients who are eligible for Medicare and Medicaid, you must attach the EOMB statement of Medicare denial to the hardcopy or upload with online submitted claim. Data submitted on the crossover claim must exactly match what was reported to and from Medicare. All paper crossover claims billed for an inpatient hospital deductible must be billed with a Bill Type 111 (Hospital Inpatient Admit through Discharge Claim).
MEDI CAL TIMELY FILING LIMIT VERIFICATION
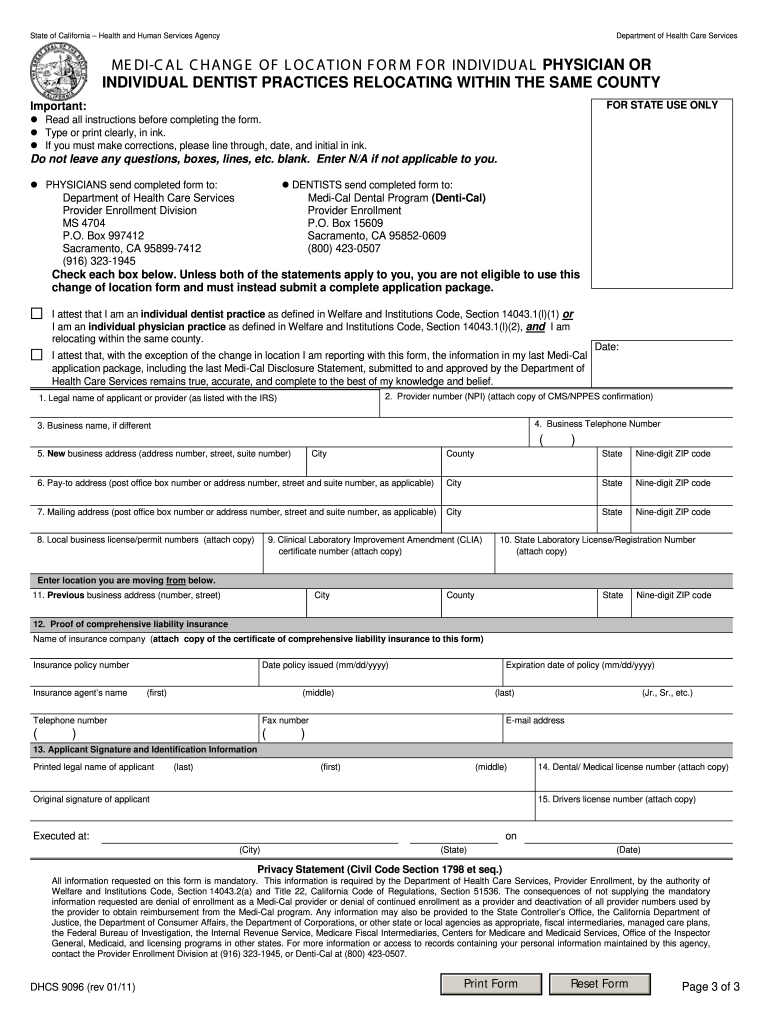
Portal users may also use the online eligibility verification tool locatedĮncouraged to maintain eligibility verification documentation, such as theĬonfirmation number obtained from the IVR or a copy of the eligibility resultsĬrossover Claims – Crossover claim forms submitted without a separate attachment for each claim will be returned to the provider.
MEDI CAL TIMELY FILING LIMIT CODE
This eight-digit code is listed on the patient’s Medical Assistance The system will then prompt you to enter the recipient This is the nine-digit number assigned to you through the Interactive Voice Response (IVR) system by calling (202) 906-8319 (in District) This information may be obtained from the Please refer to the fee schedule toĬonfirm if a PA is required. Require prior approval for reimbursement. Recipients may be enrolled in programs with Services at the beginning of each month or at each visit. Remember to utilize the Interactive Voice Response (IVR) system or the Web Portal for eligibility inquiries.Įligibility – Verify recipient eligibility for Medicaid benefits and The number entered in this field is printed on the provider's Remittance Advice. This is a 20-character field in which the provider may report an internal patient ID number, medical record number, etc. Patient Control Number Claim Field – On the UB04 claim form, the Medical Record Number field (3a), is for the provider's internal use.


 0 kommentar(er)
0 kommentar(er)
